Congenital adrenal hyperplasia
| Congenital adrenal hyperplasia | |
|---|---|
| Classification and external resources | |
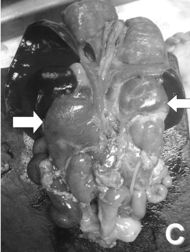 Post-mortem examination of a newborn showing adrenal hyperplasia. The enormous adrenal glands are indicated by arrows (the kidneys can be seen below them). |
|
| ICD-10 | E25.0 |
| ICD-9 | 255.2 |
| OMIM | 201910 201710 202110 201810 202010 |
| DiseasesDB | 1854 1832 4 1841 2565 |
| MedlinePlus | 000411 |
| eMedicine | ped/48 |
| MeSH | D000312 |
Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive diseases resulting from mutations of genes for enzymes mediating the biochemical steps of production of cortisol from cholesterol by the adrenal glands (steroidogenesis).[1]
Most of these conditions involve excessive or deficient production of sex steroids and can alter development of primary or secondary sex characteristics in some affected infants, children, or adults.[2] Only a small minority of people with CAH can be said to have an intersex condition, but this attracted American public attention in the late 1990s and many accounts of varying accuracy have appeared in the popular media. Approximately 95% of cases of CAH are due to 21-hydroxylase deficiency.
Contents |
Associated conditions
The symptoms of CAH vary depending upon the form of CAH and the gender of the patient. Symptoms can include:
Due to inadequate mineralocorticoids:
- vomiting due to salt-wasting leading to dehydration and death
Due to excess mineralocorticoids:
- hypertension (11beta[OH] deficiency)
Due to excess androgens:
- ambiguous genitalia, in some females, such that it can be initially difficult to determine sex
- early pubic hair and rapid growth in childhood
- precocious puberty or failure of puberty to occur (sexual infantilism: absent or delayed puberty)
- excessive facial hair, virilization, and/or menstrual irregularity in adolescence
- infertility due to anovulation
Classification
Cortisol is an adrenal steroid hormone that is required for normal endocrine function. Production begins in the second month of fetal life. Poor cortisol production is a hallmark of most forms of CAH. Inefficient cortisol production results in rising levels of ACTH, which in turn induces overgrowth (hyperplasia) and overactivity of the steroid-producing cells of the adrenal cortex. The defects causing adrenal hyperplasia are congenital (i.e., present at birth).
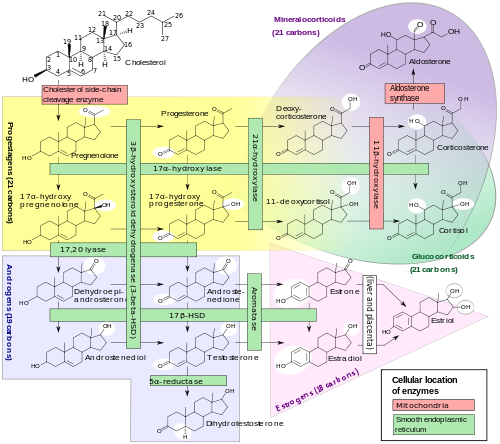
Cortisol deficiency in CAH is usually partial, and not the most serious problem for an affected person. Synthesis of cortisol shares steps with synthesis of mineralocorticoids such as aldosterone, androgens such as testosterone, and estrogens such as estradiol. The resulting excessive or deficient production of these three classes of hormones produce the most important problems for people with CAH. Specific enzyme inefficiencies are associated with characteristic patterns of over- or underproduction of mineralocorticoids or sex steroids.
| Common medical term | % | OMIM | Enzyme(s) | Locus | Substrate(s) | Product(s) | Mineralocorticoids | Androgens |
|---|---|---|---|---|---|---|---|---|
| 21-hydroxylase CAH | 90-95% | 201910 | P450c21 | 6p21.3 | 17OH-progesterone→ progesterone→ |
11-deoxycortisol DOC |
↓ | ↑ |
| 11β-hydroxylase CAH | 5% | 202010 | P450c11β | 8q21-22 | 11-deoxycortisol→ DOC→ |
cortisol corticosterone |
↑ | ↑ |
| 3β-HSD CAH | very rare | 201810 | 3βHSD II | 1p13 | pregnenolone→ 17OH-pregnenolone→ DHEA→ |
progesterone 17OH-progesterone androstenedione |
↓ | ↓ |
| 17α-hydroxylase CAH | very rare | 202110 | P450c17 | 10q24.3 | pregnenolone→ progesterone→ 17OH-pregnenolone→ |
17OH-pregnenolone 17OH-progesterone DHEA |
↑ | ↓ |
| lipoid CAH (20,22-desmolase) |
very rare | 201710 | StAR P450scc |
8p11.2 15q23-q24 |
transport of cholesterol cholesterol→ |
into mitochondria pregnenolone |
↓ | ↓ |
Since the 1960s most endocrinologists have referred to the forms of CAH by the traditional names in the left column, which generally correspond to the deficient enzyme activity. As exact structures and genes for the enzymes were identified in the 1980s, most of the enzymes were found to be cytochrome P450 oxidases and were renamed to reflect this. In some cases, more than one enzyme was found to participate in a reaction, and in other cases a single enzyme mediated in more than one reaction. There was also variation in different tissues and mammalian species.
In all its forms, congenital adrenal hyperplasia due to 21-hydroxylase deficiency accounts for about 95% of diagnosed cases of CAH. Unless another specific enzyme is mentioned, "CAH" in nearly all contexts refers to 21-hydroxylase deficiency. (The terms "salt-wasting CAH", and "simple virilizing CAH" usually refer to subtypes of this condition.) CAH due to deficiencies of enzymes other than 21-hydroxylase present many of the same management challenges as 21-hydroxylase deficiency, but some involve mineralocorticoid excess or sex steroid deficiency.
Penetrance
Further variability is introduced by the degree of enzyme inefficiency produced by the specific alleles each patient has. Some alleles result in more severe degrees of enzyme inefficiency. In general, severe degrees of inefficiency produce changes in the fetus and problems in prenatal or perinatal life. Milder degrees of inefficiency are usually associated with excessive or deficient sex hormone effects in childhood or adolescence, while the mildest form of CAH interferes with ovulation and fertility in adults.
Finally, specific problems may also differ with the genetic sex of the affected person.
Treatment
Treatment of all forms of CAH may include any of:
- supplying enough glucocorticoid to reduce hyperplasia and overproduction of androgens or mineralocorticoids
- providing replacement mineralocorticoid and extra salt if the person is deficient
- providing replacement testosterone or estrogen at puberty if the person is deficient
- additional treatments to optimize growth by delaying puberty or delaying bone maturation
- genital reconstructive surgery to correct problems produced by abnormal genital structure
All of these management issues are discussed in more detail in congenital adrenal hyperplasia due to 21-hydroxylase deficiency.
History
Before 20th century
An Italian anatomist, Luigi De Crecchio provided the earliest known description of a case of probable CAH.
I propose in this narrative that it is sometimes extremely difficult and even impossible to determine sex during life. In one of the anatomical theaters of the hospital..., there arrived toward the end of January a cadaver which in life was the body of a certain Joseph Marzo... The general physiognomy was decidedly male in all respects. There were no feminine curves to the body. There was a heavy beard. There was some delicacy of structure with muscles that were not very well developed... The distribution of pubic hair was typical of the male. Perhaps the lower extremities were somewhat delicate, resembling the female, and were covered with hair... The penis was curved posteriorly and measured 6 cm, or with stretching, 10 cm. The corona was 3 cm long and 8 cm in circumference. There was an ample prepuce. There was a first grade hypospadias... There were two folds of skin coming from the top of the penis and encircling it on either side. These were somewhat loose and resembled labia majora.
De Crecchio then described the internal organs, which included a normal vagina, uterus, tubes, and ovaries.
It was of the greatest importance to determine the habits, tendencies, passions, and general character of this individual... I was determined to get as complete a story as possible, determined to get at the base of the facts and to avoid undue exaggeration which was rampant in the conversation of many of the people present at the time of the dissection.
He interviewed many people and satisfied himself that Joseph Marzo "conducted himself within the sexual area exclusively as a male, "even to the point of contracting the "French disease" on two occasions. The cause of death was another in a series of episodes of vomiting and diarrhea.
This account, translated by Alfred Bongiovanni from De Crecchio (Sopra un caso di apparenzi virili in una donna. Morgagni 7:154-188, 1865), contains nearly all the important themes and issues. Were this man's male gender identity, role, and orientation determined by his anatomy, by his testosterone, or by his sex of rearing? His presumed female chromosomes and gonads obviously did not make him female. Yet despite his careful documentation of Marzo's unambiguous social role, De Crecchio rejects his male identity and describes him as "una donna" (Italian for "a woman"), revealing the 19th century assumption that a person's "true sex" can be determined by inspection of internal organs. Then as now, such a case prompted "undue exaggeration" and much "conversation." And then as now, we see the conflict between the desire of the scientist to learn and understand, and the sense of violation of poor Joseph Marzo's privacy. Finally, were the episodes of vomiting and diarrhea the salt-wasting of CAH?
20th and 21st century
The association of excessive sex steroid effects with diseases of the adrenal cortex have been recognized for over a century. The term adrenogenital syndrome was applied to both sex-steroid producing tumors and severe forms of CAH for much of the 20th century, before some of the forms of CAH were understood. Congenital adrenal hyperplasia, which also dates to the first half of the century, has become the preferred term to reduce ambiguity and to emphasize the underlying pathophysiology of the disorders.
Much of our modern understanding and treatment of CAH comes from research conducted at Johns Hopkins Medical School in Baltimore in the middle of the 20th century. Lawson Wilkins, "founder" of pediatric endocrinology, worked out the apparently paradoxical pathophysiology: that hyperplasia and overproduction of adrenal androgens resulted from impaired capacity for making cortisol. He reported use of adrenal cortical extracts to treat children with CAH in 1950. Genital reconstructive surgery was also pioneered at Hopkins. After application of karyotyping to CAH and other intersex disorders in the 1950s, John Money, JL Hampson, and JG Hampson persuaded both the scientific community and the public that sex assignment should not be based on any single biological criterion, and gender identity was largely learned and has no simple relationship with chromosomes or hormones. See Intersex for a fuller history, including recent controversies over reconstructive surgery.
Hydrocortisone, fludrocortisone, and prednisone were available by the late 1950s. By 1980 all of the relevant steroids could be measured in blood by reference laboratories for patient care. By 1990 nearly all specific genes and enzymes had been identified.
However, the last decade has seen a number of new developments, discussed more extensively in congenital adrenal hyperplasia due to 21-hydroxylase deficiency:
- debate over the value of genital reconstructive surgery and changing standards
- debate over sex assignment of severely virilized XX infants
- new treatments to improve height outcomes
- newborn screening programs to detect CAH at birth
- increasing attempts to treat CAH before birth
See also
- Ambiguous genitalia
- Female pseudohermaphroditism
- Adrenal insufficiency
- Androgen insensitivity syndrome
- Intersexuality
- Adrenal tumor
References
- ↑ David A. Warrell (2005). Oxford textbook of medicine: Sections 18-33. Oxford University Press. pp. 261–. ISBN 9780198569787. http://books.google.com/books?id=hL1NKQJlY1IC&pg=PA261. Retrieved 14 June 2010.
- ↑ Aubrey Milunsky; Jeff Milunsky (29 January 2010). Genetic Disorders and the Fetus: Diagnosis, Prevention and Treatment. John Wiley and Sons. pp. 600–. ISBN 9781405190879. http://books.google.com/books?id=oKCmA4dOYtMC&pg=PA600. Retrieved 14 June 2010.
 Media related to congenital adrenal hyperplasia at Wikimedia Commons
Media related to congenital adrenal hyperplasia at Wikimedia Commons
External links
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||